If you weren’t experiencing migraine during pregnancy and are suddenly having severe head pain post-baby, postpartum migraine may be to blame
The first weeks at home with a newborn are a challenging time for all new parents, but for many women, sudden, crippling migraine attacks begin after childbirth. This phenomenon is called postpartum migraine, and even though it’s extremely common, many women aren’t warned about the possibility of developing it when they become pregnant.
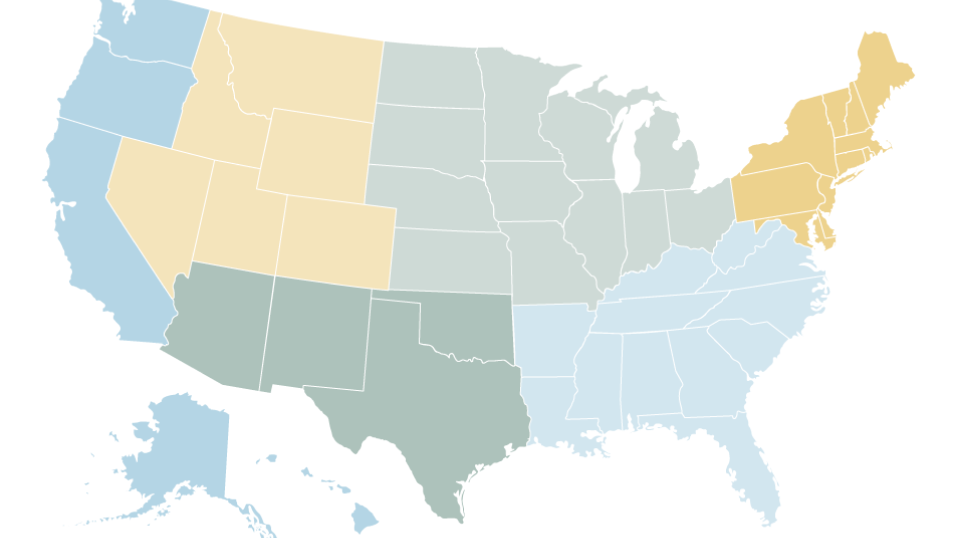
One in four of women will experience migraine within two weeks of delivery, and nearly half will have migraine attacks within the first month. “In addition to that, about 5 percent of women who have never experienced a migraine get their first one in the postpartum period,” said Dr. Angeliki Vgontzas, a neurologist at the Brigham and Women’s Faulkner Hospital. “So we’re talking about millions of women every year- that is a very high number.” Despite being so pervasive, widespread misinformation about the cause of postpartum migraine and available treatments stands in the way of an accurate diagnosis for many women.
What is Postpartum Headache?
Postpartum headache refers to the appearance or increase in headaches in women who have just had a baby, typically within the first six weeks after they deliver. Migraine in women is closely linked to hormonal changes; many women with migraine experience headache just prior to menstruation, when their estrogen levels fall, and postpartum headache is believed to reflect that same dramatic drop in estrogen levels. During the second and third trimester of pregnancy, estrogen and progesterone levels are very high, and many women who had migraine before pregnancy will find their headache symptoms lessen or disappear during this time. After delivery, both those hormones decrease dramatically, which may result in the return or first appearance of migraine.
What Factors Contribute to Postpartum Headache?
Even though there’s a unique physiology, biology behind what’s postpartum migraine, there are many environmental factors that are probably contributing as well, Vgontzas said, and the possibility of migraine after pregnancy is something moms-to-be should prepare for. “My advice to women is to discuss it with their physician even before they have their baby,” Vgontzas said.
Many of the lifestyle changes that come with a new baby are the same behaviors that can exacerbate migraine. Vgontzas lists sleep deprivation caused by infant care as a potential trigger. “Some women anecdotally will say that their headaches were a little bit worse in the postpartum period,” Vgontzas said. “That might be because they don’t have the luxury of just going into a quiet and dark room to rest or sleep.” Additionally, common migraine triggers like increased stress and missing meals are incidental for new parents and may contribute to postpartum migraine.
Treatment Options for New Moms
Many new moms worry about medications interfering with breastfeeding, but there are treatments for migraine that won’t appear in breast milk and are safe to take. Several triptans, a migraine-specific medicine, are not contraindicated for breastfeeding, and Tylenol, ibuprofen, and other NSAIDs are safe as well. Furthermore, some data suggests breastfeeding itself may reduce the frequency of migraine. “For the most part, having migraine should not change your decision about whether to breastfeed or not,” said Vgontzas. However, breastfeeding mothers should always determine whether the medications they take are excreted in breast milk and whether they are safe for infants.
For new moms experiencing migraine, the most important first step in treating their symptoms is taking them seriously, Vgontzas said. “I think most mothers focus on the wellbeing of the baby, and pay less attention to their own wellbeing during that time,” she said. “Having sleep deprivation or frequent nighttime awakenings can contribute to potentially triggering a migraine.” It is essential for new moms experiencing migraine to put their own health needs first — you can’t provide the best care for your baby when you’re trying to endure excruciating pain.
Supporting New Moms with Postpartum Headache
Supporting a new mom’s wellbeing is essential to the overall health of the family. Partners and families should help moms with migraine devise a child care plan for when a migraine attack hits, and women can work with a headache specialist to learn what symptoms precede their attacks. Staying hydrated, eating healthy meals regularly and scheduling time for relaxation is also important. Having a partner or close family member take care of nighttime feedings to help new moms maintain a normal sleeping pattern is a simple solution that can provide significant relief. Understand that postpartum migraine is real, its symptoms are severe, and women who experience it should take their health seriously and do what they need to manage the pain. “Migraine is something that women shouldn’t have to struggle with alone,” Vgontzas said.
Despite affecting so many women, little is known about the causes of postpartum migraine or how exactly hormones affect its symptoms. Dr. Vgontzas says there’s a shortage of available data and research into postpartum migraine, which limits the quality of care that headache specialists can provide. The American Migraine Foundation works to directly fund research into headache disorders and the development of new treatments to offer relief. To learn more how we’re working to improve the quality of life for the millions of Americans living with migraine, visit our Research page.