Find out more about identifying migraine symptoms and when you should talk to a doctor.
If you experience headaches that range from mild to severe intensity, you might wonder if you’re experiencing migraine. Unsure about what your symptoms mean? You’re not alone. We’ve tapped into our network of headache specialists to provide answers to common questions about migraine symptoms.
What is the difference between migraine and headache?
While some people use these terms interchangeably, there is a difference between migraine and headache.
Migraine is a brain disease. It is a clinical diagnosis, and researchers have a good understanding of the changes that occur in the nervous system during a migraine attack. It is not “just a headache.” Migraine attacks can be disabling and often includes a collection of symptoms besides head pain.
Although researchers have a good understanding of the changes that occur in the nervous system during a migraine attack, these changes are not seen on scans or in blood tests. Doctors therefore diagnose migraine based on a specific set of symptoms rather than on any test results.
Headache is a general term to describe head pain. Headache or head pain is a common symptom of migraine, but not all headaches are migraine.
How do I know if I’m having a migraine attack?
Symptoms vary from person to person. A migraine attack typically involves head pain that is moderate to severe in intensity—even unbearable. The pain is often in one area of the head (one side or both, front or back, around the eyes or behind the cheeks) and can feel like it’s throbbing or pulsating.
Other common symptoms of migraine include nausea, vomiting and sensitivity to light, sound or smells.
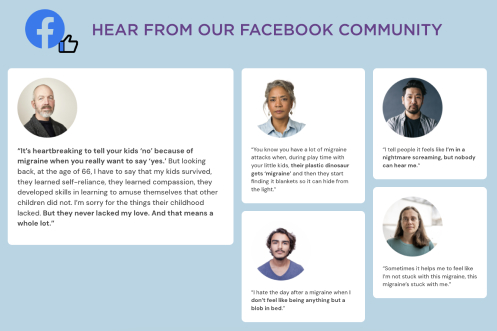
Migraine attacks can interfere with your work, school or other activities, either causing you to miss events or affecting your performance. An attack can last anywhere from four hours to several days.
The four phases of a migraine attack include prodrome, aura, headache and postdrome. Of people with migraine, 75% experience prodrome symptoms that can serve as early warning signs of an attack. Recognizing the signs of a migraine attack early can allow a person to take acute medication before the headache phase begins and help prevent, or reduce, further symptoms.
Are symptoms like dizziness, nausea and sensory sensitivity associated with migraine?
Migraine symptoms typically go beyond head pain. Nausea and vomiting are common symptoms, as well as neck pain, insomnia, anxiety or a depressed mood. Dizziness or vertigo can also be a sign of vestibular migraine.
Many people with migraine experience a heightened sensitivity to light, sound and smell. But anywhere from 40% to 70% of people with migraine have allodynia, which is pain from things that don’t usually hurt. Due to the improper processing of pain in the nervous system, this often-overlooked side effect of migraine means that something like a light touch of the skin, the brushing of hair, or even changes in temperature can feel painful to someone with allodynia.
What is aura?
Migraine attacks can occur with and without aura. Only about 25% to 30% of patients experience aura with their migraine attacks. Over time, some people may begin to experience aura without the headache phase of migraine.
Aura is most commonly visual and presents as a series of sensory disturbances that happen shortly before the headache phase of a migraine attack. These disturbances can look like blind spots, sparks, bright dots and zigzags in the visual field.
Aura can also be sensory, including symptoms such as numbness or tingling of the face, hands or feet. It can also be motor-related, although very rare it can cause weakness in parts of the body or an inability to speak clearly.
Aura usually lasts 5 to 60 minutes.
When should I be worried about migraine?
Migraine can be diagnosed as episodic or chronic, based on the number of headache days per month. People with episodic migraine have 14 or fewer headache days per month. People with chronic migraine have 15 or more headache days per month (for three or more months), with at least eight that include migraine symptoms. For some people, episodic migraine becomes chronic, which may happen if it’s not recognized and treated correctly.
If your aura or migraine is significantly increasing in frequency, it’s important to visit your physician to discuss further.
Sometimes people do need to be hospitalized for a migraine attack. If you have the worst headache of your life, especially if it comes on suddenly and reaches maximum intensity within minutes, it’s important to seek immediate medical attention to make sure it’s not a stroke or other dangerous condition.
Learn more about changes in headache patterns that could also be cause for concern.
What type of doctor should I talk to about migraine?
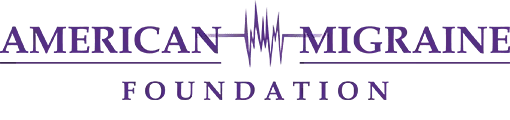
Start with speaking to your primary care provider. It may make sense to also visit a neurologist or headache specialist. You can use the American Migraine Foundation’s free tool to find a doctor.
Your doctor can be your advocate, so be open and ask questions. Know that there is hope and many treatment options to try. Prevention and acute treatment of migraine include a range of options, from supplements and prescription medications to lifestyle changes and non-medical relief strategies.
Not everyone responds the same way to medications—even to those within the same class or family of drugs. That’s why it is helpful that there are many treatment options available.
Which migraine symptoms should I track in a headache diary?
When speaking with your doctor, a headache diary can provide important information about your migraine symptoms. It can also help you recognize the early symptoms and take medication right away to relieve or prevent more intense symptoms from developing.
If you’re tracking your symptoms in a headache diary, be sure to include the location, intensity, quality and other associated symptoms, like aura, nausea, vomiting and sensitivity to light and sound. Frequency is very important for choosing which treatment options to pursue, so keep track of how many headache days—anything from mild to severe—you’re experiencing each month.
Migraine triggers can be quite individual and difficult to pinpoint. If you can, take note of what happens to your body or within your environment prior to the onset of migraine symptoms. Potential triggers can include certain foods, lighting, smells, dehydration, heat, sun, stress and a number of other factors. Also, keep in mind your lifestyle, including your sleep habits, nutrition, exercise and stress levels.
Among women, about two-thirds have menstrually related migraine. Tracking your cycle can show whether there is a relationship between your migraine attacks and the drop in estrogen at the beginning of your period or during ovulation.
Can I make lifestyle changes to avoid migraine symptoms?
Maintaining a healthy lifestyle is an important part of migraine management. Helpful lifestyle habits include a healthy diet of at least three well-rounded meals a day (as well as trying not to miss meals); staying well-hydrated with at least eight glasses of water a day; minimizing caffeine intake; getting six to eight hours of quality sleep each night; incorporating regular exercise; and managing stress with mindfulness, meditation, yoga or seeing a therapist.
While migraine symptoms aren’t always in your control, you do have the power to recognize the symptoms, seek help and work with your doctor to create a personalized plan for prevention and treatment. Migraine can be debilitating, but it’s possible to keep those symptoms from interfering with your day-to-day life.
The American Migraine Foundation is committed to improving the lives of those living with this debilitating disease. For more of the latest news and information on migraine, visit the AMF Resource Library. For help finding a healthcare provider, check out our Find a Doctor tool. Together, we are as relentless as migraine.